Archives > Volume 19 (2022) > Issue 1 > Item 09
DOI: 10.55521/10-019-109
Nancy Ellis-Ordway, LCSW, PhD
Private Practice
neomsw@mindspring.com
Virginia Ramseyer Winter, MSW, PhD
University of Missouri
ramseyerwinterv@missouri.edu
International Journal of Social Work Values and Ethics • Volume 19(1), Copyright 2022 by IFSW
This text may be freely shared among individuals, but it may not be republished in any medium without express written consent from the authors and advance notification of IFSW.
Abstract
Weight stigma is a violation of the Social Work Code of Ethics. Given that weight loss attempts have been shown to be harmful and ineffective and that they increase weight stigma, the National Association of Social Workers urgently needs to revise its response to weight loss endorsement. Social determinants of health, a robust indicator of population well-being, are ignored when interventions focus on decreasing the body size of individuals. When considering interventions, the field of social work has a responsibility to consider the evidence of what helps as well as what harms. As social workers, we need to examine our own attitudes for the biases that may harm the very people we are directed to help. The Code of Ethics gives us clear direction when applied to the topic of weight stigma.
Keywords: weight stigma, code of ethics, weight loss
The dominant discourse in our culture is the weight centered paradigm in which weight is considered a reliable measure of health, leading to the concomitant assumption that the pursuit of weight loss is a worthwhile goal that will lead to a healthier individual (Bombak, 2014). Considerable evidence refutes both ideas. The promotion of weight loss efforts contributes to weight stigma, which is associated with discrimination, oppression, and poorer health outcomes (Bacon & Aphramor, 2011). Further, the focus on changing individual body size is an effective distraction from the much larger work that needs to be done in improving social determinants of health, especially for marginalized and vulnerable populations.
Promotion of weight loss and diet culture are not common conversations in social work; however, the National Association of Social Workers (NASW) has supported programs that reinforce the weight centered paradigm (e.g., NASW, 2010: Panzer, 2020; see Figure 1), thus amplifying weight stigma. The purpose of the current paper is to explore how these efforts are a clear violation of the NASW Code of Ethics and provide recommendations for moving our field forward.
Background
Conventional thinking about weight loss is grounded in misconceptions and inaccuracies. The myths concerning weight loss include: 1) Sustainable weight loss is achievable by anyone who tries hard enough to eat less and move more; 2) Thinner people are healthier than heavier people; and 3) Losing weight makes people healthier (O’Hara & Taylor, 2018). Taken together as true, the conclusion is that people should try to lose weight and that programs promising weight loss should be promoted by anyone interested in individual and community well-being. Based on untruths, these conclusions are actively harmful (Bacon & Aphramor, 2011).
A substantial body of literature suggests that weight loss attempts almost always fail, perhaps as much as 95% of the time (e.g., Rothblum, 2018; Tylka et. al., 2014). Dieting is not only ineffective, it causes harm. Restricted eating often results in metabolic changes that lead to long term weight gain (e.g., Neumark-Sztainer et al., 2006; Ochner, et al., 2015). Weight cycling, also known as “yo-yo dieting,” is correlated to worsened mental and physical health, including body dissatisfaction, discrimination, eating disorders, death (O’Hara & Gregg, 2006), cognitive impairment, including difficulty concentrating or thinking clearly (Shaw & Tiggemann, 2004), and increased stress and cortisol levels, which are associated with heart disease, cancer, diabetes, impaired immune function and weight gain (Bangalore et al., 2017; Tomiyama et al., 2010). The assumption that weight loss results in better health outcomes is not supported by the literature (Bombak, 2014; Calogero et al., 2018; Mann et al., 2015). In fact, a compelling argument can be made that the widespread focus on losing weight and the increased stigma it engenders has contributed to the alleged “obesity epidemic” (Tomiyama et al., 2018).
Weight stigma can be defined as the devaluation and social rejection that derives from having a body that does not conform to predominant social norms or expectations regarding thinness (Tomiyama et al., 2018). It can also be thought of as weight bias, anti-fat bias or fat-phobia. It includes any-thing that devalues larger bodies or that shames or oppresses based on body size. Even the terminology we use to talk about it is questionable. The term “overweight” implies that there is a given desirable weight, and one is “over” it. The term “obese” implies pathology and is often used as a slur (Meadows & Daníelsdóttir, 2016). The unquestioned promotion of weight loss as a positive outcome and the idealizing of smaller bodies directly reinforces weight stigma. Fat-shaming is seen as a useful motivation to help encourage someone to lose weight. However, weight stigma can be considered a public health problem in its own right (Blacksher, 2018). Weight stigma may be responsible for many, perhaps most, of the health problems that have been associated with higher weights (Puhl et al., 2013; Tomiyama, et al., 2014). In fact, weight stigma is associated with 60% higher mortality risk (Sutin & Terracciano, 2017).
Weight stigma contributes to lowered engagement in the practices that promote health. Behaviors such as participating in physical activity and eating more fruits and vegetables correlate with improved health regardless of body size (Matheson et al., 2012). However, when “success” is measured by the number on the scale, such behaviors may be abandoned when they do not lead to weight loss (Thomas et al., 2015).
Weight stigma is also linked to avoidance of medical care (e.g., Puhl & Heuer, 2009). People who have been shamed at a doctor’s office because of their weight, or encouraged to embark on a weight loss effort regardless of their presenting problem, are less likely to access care in the future (e.g., DeShazo et al., 2015). Additionally, quality of care is compromised by unexamined weight stigma in medical professionals, further undermining health (Major et al., 2018).
Both anticipated and experienced stigma are associated with increased chronic stress and social isolation, and unhealthy behaviors changes (including disordered eating) which are linked with poorer health outcomes (Brochu, 2018; Hunger et al., 2018). Experiencing weight stigma is linked to hypertension, cardiovascular problems, diabetes, insulin resistance and overall impaired health (Major et al., 2013, Vartanian & Smyth, 2013). Thus, weight stigma leads to poorer health for individuals and for communities.
Children are particularly vulnerable to weight stigma, because they are growing and changing while being exposed to unrealistic images and messages in television, movies, print and social media. When well-meaning parents or others encourage youngsters to “watch their weight,” children learn that their own bodies are untrustworthy and they may embark on a lifetime of disordered eating (Wansink et al., 2017). Overvaluation of body size is a precursor of eating disorders (Stice & Van Ryzin, 2019), as is dietary restriction (Golden et al., 2016; Neumark-Sztainer et al., 2006). Given that eating disorders have the highest mortality risk of any mental illness (Harris & Barraclough, 1998), exposing children to weight stigma is dangerous to their well-being.
Meanwhile, the promotion of ineffective approaches to weight loss is highly profitable. The 66 billion dollar a year industry includes commercial weight loss programs, meal replacements, low calorie entrees, weight loss surgery, pharmaceutical products, books, DVDs, apps and online programs, profiting from the desperation of vulnerable people (Marketdata Enterprises, 2017). When these approaches do not lead to long term reduction in body size, the failure is blamed on the participant, not the product.
Assigning pathology to people in fat bodies is not only inaccurate, but it also contributes to discrimination and perpetuates oppression. Weight stigma is reinforced by all messages and assumptions that smaller bodies are better, healthier or more worthy and valuable than larger bodies. Visible fatness takes on a moral quality than leads to behaviors that are shaming and blaming towards those in larger bodies (Greenhalgh, 2012). Bias and discrimination then become justified and socially acceptable. The economic burden falls more heavily on fat women, who are paid less than their thinner peers, are less likely to be hired, or promoted (Fikkan & Rothblum, 2012), to be encouraged to attend college, or to be accepted into graduate school (Major et al., 2018). Weight stigma leads to lower socioeconomic status and greater social disparities, especially for women.
Social workers are expected to be attentive to cultural and societal forces that can negatively affect individuals and communities, especially when they contribute to oppression and discrimination in vulnerable populations. However, we are not immune to the widespread and unquestioned weight bias in our culture. Large body size is not commonly recognized as a stigmatized identity, because the concept promoted by those who profit from the dieting industry would have us believe that body size is controllable through individual effort, even though a wealth of evidence indicates that it is not (Calogero et al., 2016). Without awareness of our own unexamined assumptions, social workers with the best of intentions can inadvertently cause harm by promoting weight loss.
Social determinants are a much more robust predictor of health for individuals and communities, but are more difficult to address, involving policy, social change, funding and political will (Medvedyuk et al., 2018). The neoliberal viewpoint that weight is under individual control leads to the devaluing of large bodies and serves as a very effective distraction from addressing social determinants of health such as poverty, discrimination, oppression, housing, education, and opportunity. If we are truly interested in promoting health and well-being for individuals, families, communities and the society at large, we would do better to focus on improving lifelong learning, employment and working conditions, and minimum livable income, while addressing inequities in power, money and resources (Marmot, 2016). Decreasing disparities in access to education, employment and medical care while improving neighborhood safety and food security, for example, would be more much more beneficial than interventions focused on reducing body size.
Given the lack of quality evidence to support both the benefit of weight loss and likelihood of long-term weight loss, as well as the documented damage caused by weight cycling and stigma, ethical questions arise. The values of beneficence and non-maleficence require effective treatment benefit and an active awareness of avoiding harm, both of which are violated by promotion of weight loss (Bacon & Aphramor, 2011). A weight-centered paradigm is ineffective, harmful, and unethical (O’Hara & Taylor, 2014). There are no legitimate reasons to promote an intervention that has a history of poor outcomes and failure along with a high likelihood of iatrogenic results (Bacon & Aphramor, 2011; Bangalore et. al., 2017; Rothblum, 2018; Tylka et al., 2014). Additionally, anything that devalues larger bodies reinforces weight stigma. Support of intentional weight loss promotes the concept that smaller bodies are better, thus devaluing larger bodies.
Discussion of Ethical Considerations
The Code of Ethics of the National Association of Social Workers (2017) clearly delineates the responsibilities that social workers have to focus on improving well-being for individuals and society, with specific attention to those who are vulnerable, oppressed or living in poverty. In our focus on individual well-being in the context of society, we are especially aware of the forces in the culture and environment that can create or contribute to problems in living and our responsibility to recognize them and to address them when possible. We are charged to promote social justice by striving to end discrimination and oppression.
Weight stigma, which is implicit in any focus on weight loss, violates the Code of Ethics in a number of ways, including the core values of social justice and the dignity and worth of a person. The Code enjoins us to be aware of our own personal values and the impact they might have on ethical decision making, reminding us that our actions should be consistent with the spirit as well as the letter of the Code.
The Ethical Principles guide the work that we do, and contain several concepts to consider in the context of weight stigma. If we value the inherent dignity and worth of the person then we must consider the social injustice involved in the cultural belief that values thinner bodies over heavier ones. When weight stigma leads to discrimination, oppression and shaming, large people cannot live with dignity. If we, as social workers, are to behave honestly, responsibly and in a trustworthy manner, we must increase our knowledge in this area, learning about the evidence regarding weight and well-being instead of accepting the information that is promoted by those who stand to make a profit and promoting weight loss with our clients based on this misinformation. The Code already addresses these issues indirectly, but how do we apply the principles? The organization has a responsibility to clarify these concerns for the members. The NASW is not responsible for the individual choices made by its members, but it sets the tone and provides guidance for ethical behavior. See Table 1 for NASW Code of Ethics principles, the impact of weight stigma, and suggestions for alternative responses.
The first Ethical Standard, 1.01 (NASW, 2017), regards our commitment to our clients and our responsibility to promote their well-being. If, as we have seen, attempts to lose weight, whether in pursuit of health or to become more socially acceptable, have overwhelmingly negative outcomes, then our commitment to our clients requires that we provide them with the information needed to make better choices. Informed consent, 1.03, obliges us to explain the risks involved with weight loss attempts. Even as we respect their self-determination, 1.02, we should be aware of serious, foreseeable risk and be adequately prepared to explain said risk. Self-determination relies on informed consent.
Standard 1.04, competence, reminds us to provide services only after we have engaged in appropriate study and training. Everyone we work with makes decisions about food and eating within a cultural context so we should strive to be familiar with the relevant research. In the field of helping professions, social workers place more emphasis on understanding culture, 1.05. We are uniquely qualified to recognize the cultural valuing of bodies that contributes to inequalities, inequities, and discrimination. The cultural value of thinness not only contributes to bias and oppression in society, but to internalized shame, body dissatisfaction and impaired quality of life in individuals and families (Brochu, 2018). Our understanding of the relationship between oppression and the nature of social diversity positions us, as a profession, to be particularly sensitive to these dynamics.
Standard 1.06, conflicts of interest, is written for individuals, but applies to the organization, as well. The NASW is in conflict of interest when it promotes (Panzer, 2020) or allies in any way with organizations that directly or indirectly profit from selling weight loss (e.g., its support for the profit-oriented businesses behind “National Obesity Care Week” in October 2018; see Figure 1). It should go without saying that we should not use derogatory language, 1.12, regarding clients. However, disparaging comments about body size have become so common in our culture as to often pass unnoticed (Engeln-Maddox et al., 2012). We should be aware of, and careful about, remarks about bodies, whether the body belongs to a client, a coworker, or ourselves. Promotion or celebration of weight loss, in ourselves or others, contributes to weight stigma, as do disapproving comments about weight gain or larger bodies. Even jokes can be micro aggressions and should be avoided.
If we feel unable or unqualified to serve people in large bodies, or those with eating and body image concerns, we should refer to someone with more knowledge or expertise, per 1.16. When social workers are part of an interdisciplinary team, addressed in 2.03, we are responsible for bringing the unique social work perspective and ethics to discussion and decision-making in a way that is consistent with client well-being. Unexamined weight bias in other team members is potentially harmful to clients.
Administrators and supervisors, 3.07 and 3.08, are to advocate for adequate resources to meet client needs. This may involve continuing education and staff development to stay current with emerging knowledge regarding eating, health, body size, and weight stigma. Standards 3.09 d and e remind us that, as social workers in employment, we are expected to maintain the ethics and values of the profession by recognizing and addressing discrimination within the organization and its policies and practices.
We are reminded again in 4.01 and 5.02 that we are to stay current with emerging knowledge and base our practices on empirically tested information. When engaging in research or evaluation, we are to carefully consider possible consequences and ensure that consent is fully informed, 5.02 c and e. We must be especially vigilant regarding weight loss recommendations that focus on children, who are particularly vulnerable to the harm they can cause, and are not able to give their own consent. And, of course, we do not condone or participate in any form of discrimination, per 4.02.
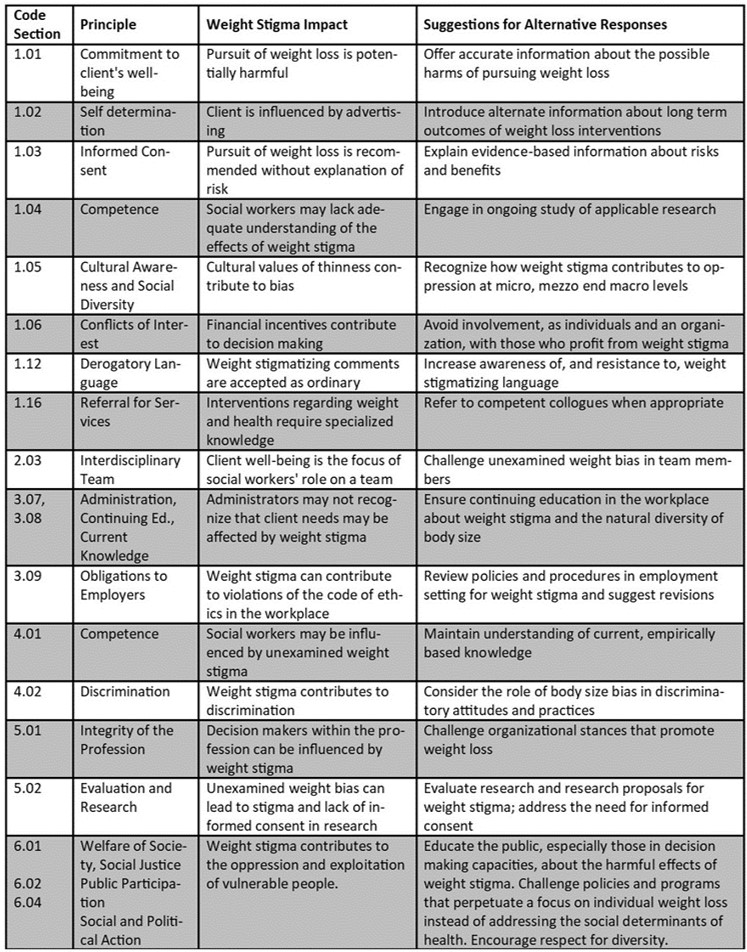
If the professional organization that represents us is acting in any way that promotes weight stigma, bias or discrimination, we are expected to speak out against it, 5.01b. As social workers, we have a commitment to promoting the general welfare of society in a way that is compatible with the realization of social justice, 6.01. This may involve facilitating the involvement of a well-informed public in shaping social policies and institutions, 6.02. If we are to promote social justice, we must encourage respect for diversity and difference in body size, ensure that all people have equal access to the resources they need to develop fully, and expand opportunity for the oppressed and those exploited by the weight loss industry, 6.04a, b and c.
Recommendations
Given the preponderance of evidence that body weight is not under individual control, that efforts to reduce body size carry considerable risk of harm, that weight stigma is a modifiable public health risk, that a focus on changing the body size of individuals distracts from more important social determinants of health, and that promotion of weight loss violates the NASW Code of Ethics, the following recommendations for the organization should be considered:
- Divest any and all involvement with organizations that profit from promoting weight loss, or are funded by corporations that do.
- Add “body size” to the list of protected categories “race, ethnicity, national origin, color, sex, sexual orientation, gender identity or expression, age, marital status, political belief, religion, immigration status, and mental or physical ability,” in sections 1.05c, 2.01b, 4.02 and 6.04d in the Code of Ethics. We accept that most of these categories, such as race, sexual orientation and age are not changeable through individual effort any more than body weight is.
- Include the category of “weight stigma” in cultural diversity courses and ethics courses in schools of social work.
- Promote continuing education courses that address the intersection of ethical issues, weight stigma, and cultural sensitivity.
- Provide social workers with resources to address weight stigma when they encounter it in agency policies, treatment teams, and other employment settings as well as in themselves.
- Develop training materials that can be used in employment and agency settings to address implicit and explicit bias based on body size.
- Promote the use of resources to identify and address internal weight bias in ourselves and with our clients.
- Carefully review existing organizational materials for weight bias and address accordingly.
Conclusion
Human bodies come in a variety of shapes and sizes. If we value human diversity in skin tones, ethnic background, gender, sex, and physical ability, we should not consider one type of body and size as more valuable or worthy than another. How do we, as individual social workers, reshape the environment for our clients to promote health, self- compassion, and self-worth instead of allowing weight stigma to mask social injustice? When we have the opportunity to influence or promote policies and interventions, we must ensure that they are compatible with the realization of equity and social justice for all people. The National Association of Social Workers and its members are uniquely qualified to stand against weight stigma. As Saleebey’s seminal 1992 article about the person-in-environment perspective reminds us, we should not become, as helpers, part of the mechanics and metaphors of oppression.
References
Bacon, Linda, & Aphramor, L. (2011). Weight science: Evaluating the evidence for a paradigm shift. Nutrition Journal, 10(1), 1–13.
Bangalore, S., Fayyad, R., Laskey, R., DeMicco, D. A., Messerli, F. H., & Waters, D. D. (2017). Body-weight fluctuations and outcomes in coronary disease. New England Journal of Medicine, 376(1), 1332–1340.
Blacksher, E. (2018). Public health and social justice: An argument against stigma as a tool of health promotion and disease prevention. In The Oxford Handbook of Stigma, Discrimination, and Health. Cary: Oxford University Press.
Bombak, A. (2014). Obesity, Health at Every Size, and public health policy. American Journal of Public Health, 104(2), e60–e67.
Brochu, P. M. (2018). Weight stigma is a modifiable risk factor. Journal of Adolescent Health, 63(3), 267–268.
Calogero, R. M., Tylka, T. L., & Mensinger, J. L. (2016). Scientific Weightism: A View of Mainstream Weight Stigma Research Through a Feminist Lens. In Feminist Perspectives on Building a Better Psychological Science of Gender. Switzerland: Springer.
Calogero, R. M., Tylka, T. L., Mensinger, J. L., Meadows, A., & Daníelsdóttir, S. (2018). Recognizing the fundamental right to be fat: A weight-inclusive approach to size acceptance and healing from sizeism. Women & Therapy, 42(1-2), 22-44.
DeShazo, R. D., Hall, J. E., & Skipworth, L. B. (2015). Obesity bias, medical technology, and the hormonal hypothesis: Should we stop demonizing fat people? The American Journal of Medicine, 128(5), 456–460.
Engeln-Maddox, R., Salk, R. H., & Miller, S. A. (2012). Assessing women’s negative commentary on their own bodies: A psychometric investigation of the negative body talk scale. Psychology of Women Quarterly, 36(2), 162–178.
Fikkan, J. L., & Rothblum, E. D. (2012). Is fat a feminist issue? Exploring the gendered nature of weight bias. Sex Roles, 66(9-10), 575-592.
Golden, N. H., Schneider, M., & Wood, C. (2016). Preventing obesity and eating disorders in adolescents. Pediatrics, 138 (3).
Greenhalgh, S. (2012). Weighty subjects: The biopolitics of the U.S. war on fat. American Ethnologist, 39(3), 471–487.
Harris, C., & Barraclough, B. (1998). Excess mortality of mental disorder. The British Journal of Psychiatry, 173(1), 11–53.
Hunger, J. M., Blodorn, A., Miller, C. T., & Major, B. (2018). The psychological and physiological effects of interacting with an anti-fat peer. Body Image, 27, 148–155.
Major, B., Mendes, W. B., & Dovidio, J. F. (2013). Intergroup relations and health disparities: A social psychological perspective. Health Psychology, 32(5), 514–524.
Major, B., Tomiyama, A. J., & Hunger, J. M. (2018). The negative and bidirectional effects of weight stigma on health. In The Oxford Handbook of Stigma, Discrimination, and Health. Cary: Oxford University Press.
Mann, T., Tomiyama, A. J., & Ward, A. (2015). Promoting public health in the context of the “obesity epidemic”: False starts and promising new directions. Perspectives on Psychological Science, 10(6), 706–710.
Marketdata Enterprises. (2017, May 4). The U.S. weight loss & diet control market. Retrieved on August 8, 2019 from https://www.marketresearch.com/Marketdata-Enterprises-Inc-v416/Weight-Loss-Diet-Control-10825677/
Marmot, M. (2016). The Health Gap, New York, NY: Bloomsbury Publishing.
Matheson, E. M., King, D. E., & Everett, C. J. (2012). Healthy lifestyle habits and mortality in overweight and obese individuals. Journal of the American Board of Family Medicine, 25(1), 9–15.
Meadows, A., & Daníelsdóttir, S. (2016). What’s in a Word? On Weight Stigma and Terminology. Frontiers in Psychology, 7.
Medvedyuk, S., Ali, A., & Raphael, D. (2018). Ideology, obesity and the social determinants of health: A critical analysis of the obesity and health relationship. Critical Public Health, 28(5), 573–585.
NASW. (2017). Code of Ethics of the National Association of Social Workers. Washington, D.C.: National Association of Social Workers.
NASW. (2010). Public comments of the NASW to the Task Force on Childhood Obesity, March 26, 2010. Retrieved on August 26, 2019 from www.socialworkers.org/LinkClick.aspx?fileticket=ar940oXaBHU%3D&portalid=0
Neumark-Sztainer, D., Wall, M., Guo, J., Story, M., Haines, J., & Eisenberg, M. (2006). Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? Journal of the American Dietetic Association, 106(4), 559–568.
Ochner, C. N., Tsai, A. G., Kushner, R. F., & Wadden, T. A. (2015). Treating obesity seriously: When recommendations for lifestyle change confront biological adaptations. The Lancet Diabetes & Endocrinology, 3(4), 232–234.
O’Hara, L., & Gregg, J. (2006). The war on obesity: A social determinant of health. Health Promotion Journal of Australia, 17(3), 260–263.
O’Hara, L., & Taylor, J. (2014). Health at Every Size: A weight-neutral approach for empowerment, resilience and peace. International Journal of Social Work and Human Services Practice, 2(6), 272–282.
O’Hara, L., & Taylor, J. (2018). What’s wrong with the ‘war on obesity?’ A narrative review of the weight-centered health paradigm and development of the 3C framework to build critical competency for a paradigm shift. SAGE Open, 8(2), 1-28.
Panzer, B. (2020, February). Childhood Obesity: Social work and the epidemic. Social Work Advocates, 8-9.
Puhl, R., Peterson, J. L., & Luedicke, J. (2013). Fighting obesity or obese persons? Public perceptions of obesity-related health messages. International Journal of Obesity, 37(6), 774–782.
Puhl, R. M., & Heuer, C. A. (2009). The stigma of obesity: A review and update. Obesity, 17(5), 941–964.
Rothblum, E. D. (2018). Slim chance for permanent weight loss. Archives of Scientific Psychology, 6(1), 63–69.
Saleebey, D. (1992). Biology’s challenge to social work: Embodying the person-in-environment perspective. Social Work, 37(2), 112-118.
Shaw, J., & Tiggemann, M. (2004). Dieting and working memory: Preoccupying cognitions and the role of the articulatory control process. British Journal of Health Psychology, 9(2), 175–185.
Stice, E., & Ryzin, M. J. V. (2019). A prospective test of the temporal sequencing of risk factor emergence in the dual pathway model of eating disorders. Journal of Abnormal Psychology, 128(2), 119–128.
Sutin, A. R., & Terracciano, A. (2017). Perceived weight discrimination and high-risk health-related behaviors. Obesity, 25(7), 1183-1186.
Thomas, D. M., Kyle, T. K., & Stanford, F. C. (2015).The gap between expectations and reality of exercise-induced weight loss is associated with discouragement. Preventive Medicine, 81, 357-360.
Tomiyama, A. J., Mann, T., Vinas, D., Hunger, J. M., Dejager, J., & Taylor, S. E. (2010). Low calorie dieting increases cortisol. Psychosomatic Medicine, 72(4), 357–364.
Tomiyama, A. J., Epel, E. S., Mcclatchey, T. M., Poelke, G., Kemeny, M. E., Mccoy, S. K., & Daubenmier, J. (2014). Associations of weight stigma with cortisol and oxidative stress independent of adiposity. Health Psychology, 33(8), 862–867.
Tomiyama, A. J., Carr, D., Granberg, E. M., Major, B., Robinson, E., Sutin, A. R., & Brewis, A. (2018). How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Medicine, 16(1).
Tylka, T. L., Annunziato, R. A., Burgard, D., Daníelsdóttir, S., Shuman, E., Davis, C., & Calogero, R. M. (2014). The weight-inclusive versus weight-normative approach to health: Evaluating the evidence for prioritizing well-being overweight loss. Journal of Obesity, 2014, 1-18.
Vartanian, L. R., & Smyth, J. M. (2013). Primum non nocere: Obesity stigma and public health. Journal of Bioethical Inquiry, 10(1), 49–57.
Wansink, Brian, Lara A. Latimer, and Lizzy Pope. (2017). “Don’t eat so much:” How parent comments relate to female weight satisfaction. Eating and Weight Disorders, 22(3), 475–81.